Assessing bait acceptance of local dogs, oral rabies vaccination success and human contact risk in Bali, Indonesia
Abstract
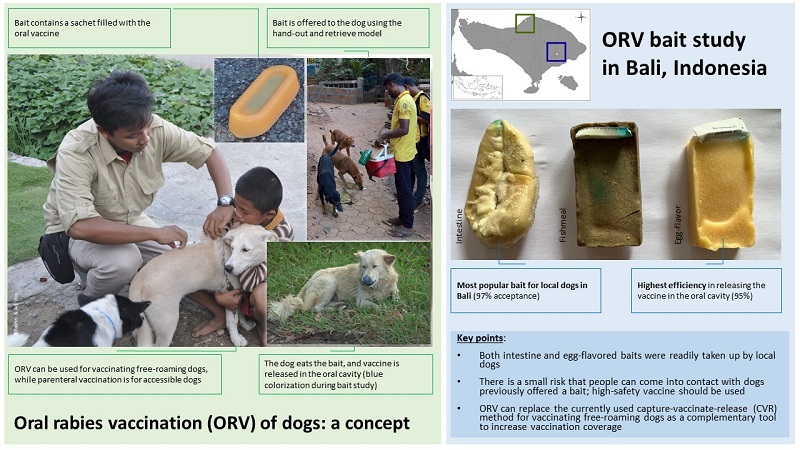
Aim: The objective of this study was to identify the preferred bait of local dogs in Bali and estimate oral rabies vaccination (ORV) success in locations with varying geographic and demographic conditions. In addition, an evaluation of potential direct and indirect contact with the placebo sachet contents was conducted.
Methods: The study was a randomized controlled trial conducted in two pilot areas of Bali using imported and hand-made baits. All dogs were offered a single bait containing a sachet of blue-dyed water using the “hand-out and retrieve” technique. Several methods were used to determine the likelihood of contact with the placebo vaccine. Comparing ORV with capture-vaccinate-release (CVR) methods, field officers were given Google Forms questions to answer. Statistical analysis was performed using univariate contingency table testing, followed by the development of a multiple logistic regression (MLR) model.
Results: With 96.9% acceptance, intestine was the most popular bait for local dogs in Bali, and egg bait came in second (81.1%). However, the egg bait was 95.2% effective in releasing the vaccine in the oral cavity, followed by the intestine at 82.6%. 6.1% of surveyed households had direct contact with a dog that had recently consumed a vaccine bait. A survey among field officers also indicated that they preferred ORV over CVR, as the former is more suitable for vaccinating inaccessible dogs and less stressful for the teams and the animals.
Conclusion: In Bali, both a locally-made intestine bait and an industrially-produced egg-flavored bait were readily taken up by local dogs. There is a small risk that people can come into contact with dogs previously offered a bait; hence, only vaccines with a high safety profile should be used. ORV can replace the currently used CVR method for vaccinating free-roaming dogs as a complementary tool to increase vaccination coverage.
Keywords
INTRODUCTION
Rabies has been reported in Indonesia since the 1880s[1] when the first case of rabies was reported by Schoorl from a horse in Batavia (modern Jakarta)[2]. Subsequently, regulations for controlling and eliminating rabies were implemented by the Dutch East Indies colonial government. After this initial case, rabies outbreaks spread to almost all major islands of Indonesia[3]. Over time islands that remained historically free of rabies have become infected. Spread has continued and in the last 15 years, more islands have become infected with rabies, including Bali (2008), Nias (2010), Larat (2010), Dawera (2012), and Sumbawa (2019)[4].
The Government of Indonesia (GoI) has committed itself to a rabies elimination program with a target of Indonesia becoming free of canine-mediated human rabies by 2030, and in so doing, is in alignment with the global target of rabies elimination[5]. To achieve this target, GoI is adopting a mass dog vaccination (MDV) strategy with a minimum vaccination coverage of 70%[4]. The success story of MDV implementation can be seen in Bali where in the first years of the campaign, the results achieved were entirely satisfying, especially the success in reducing the incidence of cases in animals in the following years[6].
Despite MDV being shown to be the single most cost-effective strategy for controlling canine-mediated rabies[7], implementing effective MDV in Indonesia is very problematic[8]. A number of obstacles to controlling rabies in Indonesia have been identified including difficulties in achieving effective MDV with high rates of vaccine coverage, vaccine distribution to remote areas, socio-cultural attitudes, and lack of resources[9]. In addition, the large number of hard to handle free-roaming dogs, even though many have owners, also pose a big challenge for rabies elimination as they cannot be easily captured and restrained for vaccination[10]. Several initiatives have been carried out in areas severely affected by rabies, such as Flores, Nias, and Bali, and these have shown promising results, but rabies continues to occur[4].
GoI is facing a major challenge to meet the zero by 2030 target without revising the strategy for rabies control and elimination and improving program delivery. It is well-accepted that vaccination must target the dog populations which act as reservoirs in the rabies virus transmission cycle[11]. Parenteral MDV with high-quality rabies vaccines is preferred for populations of dogs that are accessible[12]. More problematic is handling free-roaming dogs as it can be very difficult to reach these for vaccination. In Bali, the government continues to use parenteral vaccination and employs teams of dogcatchers to overcome this issue at a considerable cost in terms of time and workforce. Oral rabies vaccination (ORV) has the potential to reach these dogs and increase vaccination coverage[4].
ORV has been successful in achieving high vaccination coverage in free-roaming dog populations in India[13], the Philippines[14], and Haiti[15] and has been instrumental in eliminating wildlife-transmitted rabies in Western Europe[16]. One of the preconditions to the success of ORV is the selection of suitable bait - as essential as identifying a safe and efficacious vaccine. One of the characteristics of baits to be used for effective ORV administration is that they must be attractive to the target population, accepted culturally, and able to be produced in sufficient quantities[13]. Bait trials had previously been conducted in Indonesia, specifically in East Flores Regency, Flores Island, to determine the preferences of local dogs for the type of baits used. The result of the study showed that locally made fishmeal baits were preferred over commercial baits. However, this study only focused on bait acceptance and did not assess vaccine release and delivery[17]. The present study aimed to identify the preferred bait of local dogs in Bali using low-cost baits and to estimate oral vaccination success in locations with different geographic and demographic conditions. Further, an assessment of potential direct and indirect human contact with the contents of the placebo sachets was carried out.
MATERIALS AND METHODS
Study setting and design
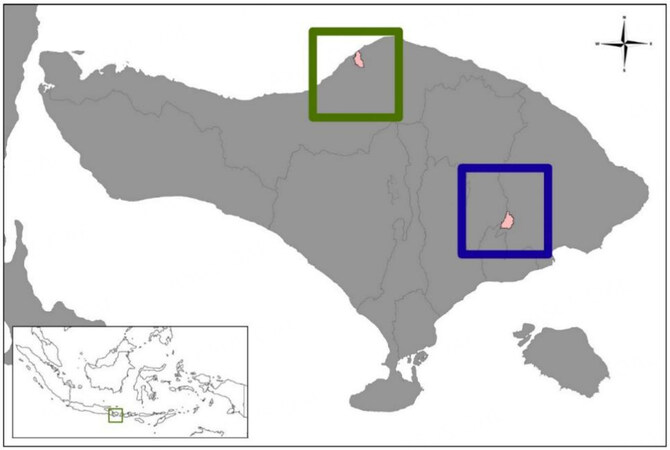
The study was designed as a controlled-randomized research study and conducted in two pilot areas in Bali Province, namely Nongan village, Karangasem District represents rural areas (November 23-25, 2021), and Banyuning village, Buleleng District, which represents urban areas (November 30 to December 2, 2021) [Figure 1].
Figure 1. Location of Nongan village, Karangasem (blue square) and Banyuning village, Buleleng (green) in Bali Island where the bait acceptance study was conducted.
Prior to the study, 10 teams of two people from these districts were trained on how to approach a dog, offer bait to the targeted animals, and fill out the recording form. This study used two types of imported manufactured baits made from fishmeal and egg powder, and one locally hand-made bait using Bali cattle intestine [Table 1]. The intestine bait, as a positive control, has previously shown very high acceptance rates in different settings, including the Philippines[18], Bangladesh[19], Thailand[20], and Navajo Nation (USA)[21].
Comparison of bait specifications during the bait study in Bali, Indonesia
| Type | Fishmeal | Egg-flavored + paste | Boiled intestine |
| Description: | Fish | Egg | Intestine |
| Size (cm): | 8.5 × 4.0 × 1.2 | 8.5 × 4.0 × 1.2 | 10-15 long |
| Weight (gr): | 43.0 | 43.0 | 15-25 |
| Composition (major components): | Fish meal, vegetable fat | Whole egg powder, gelatine | 10-15cm long sections of boiled Bali cow intestine |
| Storage conditions: | ≤ 0 °C | ≤ 0 °C | ≤ 0 °C |
| Transport conditions: | frozen | frozen | frozen |
As a negative control, machine-made fishmeal-based bait was used. The fishmeal bait has been used extensively in Europe during oral vaccination campaigns targeted at foxes and raccoon dogs[22-24]. Although this bait is highly attractive for these animals, it has been shown to be less well accepted by dogs[18,25,26].
A newly developed egg-flavored bait was also tested[27] with the addition of commercial wet dog food paste with beef flavor. This bait has shown almost similar acceptance rates to dogs as boiled-intestine bait[20]. During a systematic program working through the study area, all dogs observed were offered a single bait; the bait type offered was pre-determined using a randomization list. All three bait types contained a sachet filled with 3.0 mL of blue-dyed water. The colorant used, Patent Blue V (Thermo Fisher Scientific, Geel, Belgium), is safe and commonly used in food products.
Procedures
Prior to the bait acceptance study, public awareness was raised by informing the village government, traditional elders, and the community in the village where the activity was located. The information provided covered the concept of the oral rabies vaccination method and the study to be conducted in their area. The different bait types were taken from the freezer at the storage site in the field study area in cool boxes containing ice packs. The baits were thawed before offering them to the dogs [Figure 2A].
Figure 2. (A) Different baits used (left: boiled intestine; middle: fishmeal; right: egg-flavored); (B) the appearance of blue coloration of the oral cavity and tongue.
A two-person team visited the assigned study sites using a motorcycle and systematically searched for dogs between 07:00 and 17:00, preferably early morning and late afternoon. The team leader was responsible for determining which bait type would be offered to the dog encountered (according to the randomization list), for filling out the animal registration and treatment record form as well as informing dog owners or other persons present on the purpose of the study, and also answering any other questions raised by the bystanders. A leaflet was available for interested bystanders, including a phone number that the public could use for questions or reporting incidents such as adverse events. The other person offered the bait to the dog, closely observing bait acceptance, bait puncturing (release of dye) and provided additional support to the team leader. This person also collected any baits not accepted and the discarded vaccine sachets.
The animal registration and treatment record form were filled out for every baiting attempt, including attempts where dogs refused the bait. The general assessment of the acceptance of each bait was based on a number of variables, including whether the targeted dog showed interest or ignored the bait, the estimated quantity of bait consumed, and the consumption or chewing time of each bait. An assessment of the potential for efficient vaccine release from each bait type was also carried out by looking at whether the sachet was perforated or not by the dog. In addition, an estimation of the success of oral vaccination in the targeted dogs was also determined during this study based on defined variables, such as the release of the placebo due to chewing, indicated by the appearance of blue coloration of the oral cavity and tongue [Figure 2B]. See Table 2 for the list of parameters used during the study.
Parameters used during bait acceptance study in Bali, Indonesia
| Parameter | Test | Assessment | |
| Bait handling | Interest | Observation | Direct contact (nose, mouth) with bait |
| Consumption | Observation | Bait was (partially/fully) consumed | |
| Handling time | Observation | Time (sec.) between offering the bait and the end of bait handling | |
| Sachet handling | Perforation | Observation | If the sachet has been perforated or not |
| Discarded | Observation | If the sachet has been discarded or not | |
| Oral vaccination success | Observation | Based on bait handling, it will be assessed if the liquid inside the sachet has been released within the oral cavity | |
Additional information recorded for each dog included ownership, dog supervision, sex, age, size, and whether individuals in the community contacted the placebo vaccine during and/or after bait distribution.
Human risk
To assess the potential for contact between persons and the contents of the bait, a number of methods were used during and following the bait acceptance study. At the time of offering the baits, officers were vigilant to note if there was any contact with the placebo vaccine either by dog owners or bystanders. A house-to-house survey was also conducted on days 2 and 3 to ask owners whether they or household members had contact with their dog when its tongue was still blue as a result of baiting. If applicable, the type of contact (whether it was a lick or a bite) and which body part was contacted was recorded. Coordination with the local public health center was also carried out to obtain information related to blue-tongued dog contact during the study until the end of the week as a source of additional information.
Field staff questionnaire
Questions using Google Forms were given to all field officers involved comparing ORV with CVR using nets to target free-roaming dogs. Field staff questioned were dog catcher team members and district veterinarians, as well as rabies vaccination master trainers from staff at central, provincial, and district governments. Respondents were asked what they liked or disliked about the ORV and CVR methods, what suggestions they would make to improve these methods, as well as their opinion on which method was the most preferred, and which was the best when it came to vaccinating free-roaming dogs also considering animal welfare issues. The questionnaire aimed to support decision making in optimising future mass vaccination strategies for dogs in Indonesia.
Statistical analysis
Statistical analysis was performed using univariate contingency table testing (Chi² - and Fisher’s exact test), followed by the development of a multiple logistic regression model (MLR). The dependent variable was determined as “vaccination success”; defined by the release of the contents of the sachet in the oral cavity (yes/no). Independent variables were bait type, date, period of the day, day of the campaign, study area, and team. As weather conditions can affect the behavior of dogs and subsequent bait handling, the date was also taken as a variable. The period of the day impacts the activities of dogs, so this was also included with the day being divided into four periods; early morning (06:00-09:59), late morning (10:00-12:59), early afternoon (13:00-14:59), and later afternoon (15:00-18:00). As the teams gained experience in approaching and offering bait to the dogs during the campaign, the day of the campaign in the two districts was also considered as a variable: 1st, 2nd, and 3rd day. The effect of the two different districts (urban, rural) and the 10 different teams was included. Additional variables on when and where the dog was offered a bait were also included in the statistical analysis - level of confinement, if the dog was alone or together with other dogs, ownership status, size, gender, and age. Variables with P ≤ 0.20 were included in the final MLR model. Statistical analyses were carried out using GraphPad Prism v9.0 (GraphPad Prism Software Inc., San Diego, USA).
RESULTS
Of the 1,000 targeted dogs, 500 in each district, 6% were identified as restricted dogs, and the other 94% were free-roaming dogs. 70% of target dogs were owned, 27% were ownerless, and the rest were with unknown ownership status. 69% of target dogs were male, and 30% of dogs were female. 84% of target dogs were adults, 15% were juveniles, and the rest were puppies.
The earliest and latest time point a dog was offered a bait was 06:30 and 17:07. Most dogs were approached during the early morning (06:00-09:59). Of the 1,000 dogs approached, 781 (78.1%) showed interest in the bait offered, 211 (21.1%) dogs ignored it, and from 8 (0.8%) dogs no information was available. Almost all dogs that showed interest in bait subsequently consumed it.
However, there was a significant difference among the different bait types offered [Table 3]. Dogs showed the highest interest in the intestine bait (96.9%), followed by the egg bait (81.1%), and only 59.5% of the dogs were interested in the fish meal bait. In case the animals consumed the bait, the egg bait was more efficient in releasing the vaccine in the oral cavity than the intestine bait: 95.2% and 82.6%, respectively. Also, here the fish meal bait performed poorly (69.6%).
Number and percentage of dogs that were interested and subsequently consumed and considered vaccinated per bait type
| Factor | Intestine | Egg | Fishmeal | |||
| % | n | % | n | % | n | |
| Offered | 100 | 327 | 100 | 317 | 100 | 348 |
| Interested | 96.9 | 317 | 81.1 | 257 | 59.5 | 207 |
| Consumed (if interested) | 99.7 | 316 | 98.8 | 254 | 99.5 | 204 |
| Vaccinated (if consumed) | 82.6 | 256 | 95.2 | 239 | 69.6 | 135 |
| Vaccinated (if offered) | 78.3 | 256 | 75.4 | 239 | 38.8 | 135 |
Dogs offered a fish meal bait were significantly less often considered vaccinated than the other two bait types. The only other variable showing a significant effect was the team involved [Table 4].
Vaccination success defined as the release of the sachet contents in the oral cavity of the dog for the different factors and their settings; n - number of dogs considered vaccinated, N - number of dogs offered a bait. The different settings of each variable were compared with each other for significant differences
| Factor | Settings | Vaccination success | P-value | Test | |
| n/N | % | ||||
| Age | Juvenile | 95/145 | 65.5 | 0.13 | Fisher’s |
| Adult | 528/840 | 62.9 | |||
| Area | Karangasem | 308/500 | 61.6 | 0.40 | Fisher’s |
| Buleleng | 322/500 | 64.4 | |||
| Bait | Intestine | 256/330 | 78.3 | < 0.0001 | Chi2 |
| Egg | 239/319 | 75.4 | |||
| Fish meal | 135/351 | 38.8 | |||
| Campaign day | 1st | 258/426 | 60.6 | 0.36 | Chi2 |
| 2nd | 243/378 | 64.3 | |||
| 3rd | 129/196 | 65.8 | |||
| Confinement | Restricted | 40/58 | 69.0 | 0.40 | Fisher’s |
| Free-roaming | 591/941 | 62.8 | |||
| Date | 23.11.2021 | 115/205 | 56.1 | 0.33 | Chi2 |
| 24.11.2021 | 151/234 | 64.5 | |||
| 25.11.2021 | 42/61 | 68.9 | |||
| 30.11.2021 | 142/221 | 64.7 | |||
| 01.12.2021 | 92/144 | 63.9 | |||
| 02.12.2021 | 87/135 | 64.4 | |||
| Ownership | Owned | 449/707 | 63.5 | 0.46 | Fisher’s |
| Ownerless | 162/266 | 60.9 | |||
| Period | Early morning | 220/356 | 61.8 | 0.82 | Chi2 |
| Late morning | 213/330 | 64.5 | |||
| Early afternoon | 151/244 | 61.9 | |||
| Late afternoon | 46/70 | 65.7 | |||
| Sex | Male | 424/689 | 61.5 | 0.58 | Fisher’s |
| Female | 201/301 | 66.8 | |||
| Size | Small | 25/34 | 73.5 | 0.13 | Chi2 |
| Medium | 402/658 | 61.1 | |||
| Large | 203/306 | 66.3 | |||
| Social status | Single | 439/680 | 64.6 | 0.16 | Fisher’s |
| Multiple | 191/319 | 59.9 | |||
| Team | I | 49/100 | 49.0 | 0.0005 | Chi2 |
| II | 63/100 | 63.0 | |||
| III | 75/100 | 75.0 | |||
| IV | 65/100 | 65.0 | |||
| V | 56/100 | 56.0 | |||
| VI | 55/100 | 55.0 | |||
| VII | 77/100 | 77.0 | |||
| VIII | 60/100 | 60.0 | |||
| IX | 62/100 | 62.0 | |||
| X | 68/100 | 68.0 | |||
For the MLR analysis, the following variables included bait type, team, social status, size, and age of the dog, as the estimated p-value in the univariate analysis was < 0.20. Ten dogs were removed from the data set as no data were available on sex. The estimated Odds Ratios of the MLR model are shown in Table 5. Several teams were more likely to successfully vaccinate dogs approached than the reference team I. Fish meal bait was also significantly less suitable than the other two baits. The vaccination success was higher for smaller-sized dogs, but the likelihood that female dogs were more often successfully vaccinated was not significant. Finally, there was also no significant effect on the outcome of the vaccination attempt if the dog was alone or with other dogs when the bait was offered.
The Odds Ratio and the Confidence Interval of the Multiple Logistic Regression Model; as a reference, Team I, fish meal bait, multiple dogs, medium-sized dogs, and males were selected
| Variable | Odds ratio | 95%CI |
| Team II | 1.99 | 1.08-3.73 |
| Team III | 3.29 | 1.68-6.57 |
| Team IV | 1.94 | 1.03-3.68 |
| Team V | 1.61 | 0.88-2.97 |
| Team VI | 1.33 | 0.70-2.56 |
| Team VII | 3.64 | 1.78-7.58 |
| Team VIII | 1.84 | 0.94-3.62 |
| Team IX | 1.85 | 0.97-3.56 |
| Team X | 2.13 | 1.10-4.18 |
| Bait - intestine | 5.67 | 4.03-8.06 |
| Bait - egg | 4.94 | 3.51-6.70 |
| Social - single | 1.15 | 0.84-1.57 |
| Size - large | 0.98 | 0.66-1.45 |
| Size - small | 2.44 | 1.06-6.05 |
| Sex - female | 1.28 | 0.92-1.79 |
Details on bait handling by the dogs are summarized in Table 6. The intestine bait was significantly more often completely consumed than the other two bait types. The handling time of the intestine bait was significantly shorter than for the other two baits. The sachet inside the intestine bait was significantly more often swallowed than for the egg - and fish meal baits. However, the sachet in the egg bait (95.9%) was significantly more often perforated than the sachet inside the intestine bait (84.9%) and fish meal bait (71.1%). The bait handling time was not influenced by the fact that other dogs were present when the bait was offered.
Bait handling per bait type- only when the bait was accepted and consumed; N - number of dogs observed that were offered and consumed a bait for the listed setting
| Factor | Settings | N | Bait type (%) | Test | ||
| Intestine | Egg | Fish | ||||
| Amount consumed | 100% | 83 | 91.0 | 69.0 | 64.1 | Chi2 |
| 50%-99% | 93 | 4.8 | 13.7 | 22.2 | ||
| < 50% | 581 | 4.2 | 17.3 | 11.0 | ||
| Sachet-1 | Perforated | 618 | 84.9 | 95.9 | 71.1 | Chi2 |
| Sachet-2 | Discarded | 513 | 41.0 | 83.7 | 93.3 | Chi2 |
| Swallowed | 233 | 59.0 | 16.3 | 6.7 | ||
| Handling time | Very short (< 10 sec) | 89 | 19.6 | 9.7 | 2.0 | Chi2 |
| Short (10-30 sec) | 224 | 32.8 | 27.4 | 27.4 | ||
| Medium (31-60 sec) | 187 | 19.3 | 26.2 | 31.5 | ||
| Long (> 60 sec) | 256 | 28.3 | 36.7 | 39.1 | ||
During the bait acceptance study, 10 contacts with the vaccine baits by the dog owners or caretakers were observed. None of these contacts led to direct contact with the contents of the sachet, as indicated by the absence of visible blue staining. Also, no biting incident was reported from a dog in the study areas to the Public Health authorities during 3 days following the study. A total of 375 households were visited during the second and third day afternoon following a visit in the morning where the dog had been offered a bait; 125 in Karangasem and 250 in Buleleng. A total of 23 contacts between blue-tongued dogs and a household member were reported. All contacts concerned licking incidents; 11 - hands only, 8 - hands and feet, 3 feet only, 1 - hand and cheek. Hence, in 6.1% of the household surveyed, someone had direct contact with a dog that recently consumed a vaccine bait.
A detailed comparison of the opinions of field officers regarding the advantages and disadvantages of ORV and CVR is provided in Table 7. In general, more than two-thirds of respondents (17 of 24) preferred the oral vaccination method to the parenteral using nets to capture free-roaming dogs, 3 people preferred the netting method, and the remaining did not prefer one method over the other. The reasons for choosing the oral vaccination method include that it is easier to do, more humane as it does not stress dogs, is more efficient because it requires less manpower, can reach dogs that are difficult to handle, and is more fun. Some people prefer to vaccinate dogs using nets because they believe that once a dog has been captured, it can be vaccinated with certainty, the method is quicker to administer, and they are accustomed to using it. In addition, 16 people (67%) estimated the oral method could reach and vaccinate more dogs, while 25% thought netting vaccination was superior in this regard. Considering animal welfare, 17 people (71%) judged the oral method as better, 4 people (17%) rated vaccination using nets as better, and the rest assessed both methods equally.
Assessment of staff involved in the study regarding the advantages and disadvantages of each vaccination method: oral vaccination and parenteral vaccination using nets targeting free-roaming dogs
| Vaccination methods | Advantages | Disadvantages |
| Oral vaccination | Easy to do | Takes a longer time to implement* |
| Could reach and vaccinate free-roaming dogs | Difficulties in feeding a group of dogs | |
| Low risk of getting bitten | Some dogs swallow bait directly without chewing | |
| Requires little equipment | Owners or local residents have concerns about this new method | |
| More fun | There are no universally suitable baits | |
| Capture-vaccinate-release (CVR) method | Dogs must be vaccinated if they are caught | Dogs escape before being caught due to previous campaign trauma |
| Fast vaccination | Heavy net to carry around | |
| Easy to catch the dogs | Difficult to implement* | |
| Guaranteed team safety | Spreading skin diseases | |
| Easy vaccine application | Requires huge human resources and costs |
DISCUSSION
Selecting a bait that is well accepted by the local dog population and allows the release of the vaccine in the oral cavity is essential for the effective ORV of dogs. Therefore, comparative bait acceptance studies have been carried out in many countries[18,25,28-32]. Due to dissimilarities in study design, it is not easy to directly compare the results obtained among these studies. To reduce this, similar study protocols as have been applied elsewhere were used in the present study with a small difference in bait - and sachet types used[20-21]. In comparison, for example, in Thailand, the intestine bait was slightly adapted, with pieces of boiled intestine placed inside a collagen casing[20]. The high attractiveness of the intestine bait, as observed in other studies[18,20,21,33], was confirmed in Bali; 96.9% of the dogs showed interest in the bait when it was offered directly. The slightly lower observed interest in the egg-bait (81.1%) lies within the range observed in other countries; 77.4%-95.8%[20,21,27,33,34]. As these local free-roaming dogs are often fed leftovers, the animals are familiar with locally available material that can be used for bait preparation. The texture, smell, and taste of industrially manufactured baits like egg - and fish meal baits may be unfamiliar, and thus the animals are less inclined to accept these readily. To overcome this, a locally available pet liquid snack was pasted on the external egg bait matrix since, in Thailand, it was shown that such a substance improved bait acceptance[34]. Here, adding paste to egg bait accelerated bait acceptance when offered to the dogs, resulting in an increase in bait acceptance from 87.3% (without paste) to 92.8% (with paste)[34]. Only 58.6% of the dogs offered the fish meal bait consumed it, similar to Thai dogs (50.3%) but lower than dogs in Navajo Nation (81.8%)[20-21]. Also, in Turkey, it was shown that the fish meal bait, as used for ORV of foxes and raccoon dogs in Europe, was not very attractive to local dogs[28].
Bait acceptance is only one part of the requirement for the effective use of ORV. For ORV to be successful, the contents of the sachet must be released in the oral cavity, where it will enter the body via the mucous membrane and tonsils[35]. In this and related bait acceptance studies, vaccination success was assessed by bait handling and, if possible, visible staining of the oral cavity with the blue dye from the sachet[20,21,27,36]. The validity of this approach has been previously confirmed by the presence of detectable antibodies during serological studies when dogs were offered vaccine-loaded intestine - or egg baits[33,37,38].
As has been observed in Thailand[20,34], the estimated vaccination success of the egg bait was higher after bait consumption than that of the intestine bait, partially compensating for the lower bait acceptance. Therefore, it seems that the egg bait with or without local optimization (pet food paste/gravy) is an excellent bait candidate achieving high vaccination rates in different settings all over the world, including Bali. The use of a mass-producible vaccine bait has many additional advantages over baits made from local-available material, including consistent quality and availability[34]. The results obtained were in agreement with previous studies using the same protocol. A significant effect on vaccination success was identified for the different vaccination teams, ranging from 49% to 77%. A similar observation was made in Goa State, India[27]. It is not clear if the observed differences were caused by behavioral aspects of the vaccinators, such as how they observed and approached the dogs, or if it was a result of variation in their assessment of bait handling and subsequent “vaccination” success. There was no significant effect observed on vaccination success against the increased experience of the teams taken over the 3 consecutive study days. Although the vaccination success increased every day, most likely, the period was too short to have any significant effect. In Turkey, a noticeable difference was found between a highly experienced team and inexperienced teams consisting of veterinary students[39]. The observed higher vaccination success in smaller-sized dogs was also seen in Thailand[20]. Bait acceptance and subsequent vaccination success were not influenced by the time of bait offering, similar to the studies in the Navajo Nation, India, and Thailand[20,21,27].
One of the requirements of the World Organisation for Animal Health (WOAH) concerning the use of ORV is a risk assessment for human safety and the likelihood of human contact with the vaccine virus[40]. The risk assessment for human safety is not only influenced by the vaccine but also by the bait distribution system. The system used during these bait acceptance studies is similar to the suggested hand-out and retrieve model as practiced in Thailand[34]. The baits were offered directly to the dogs encountered, and any bait not accepted was retrieved by the vaccinators. Furthermore, all discarded sachets were also collected, thus reducing potential human contact with the bait considerably[41-42]. Another bait distribution system proposed is handing out baits to dog owners at temporary bait delivery sites. During a field study, it was shown that this method resulted in a high number of unintentional contacts with the baits; 1.7% of all inhabitants claimed to have had contact with the baits during a subsequent survey, including a child putting the bait in its mouth[43]. In another study, baits were placed along transects to be located by dogs themselves, similar to the approach used for wildlife. Here, 1.4% of the inhabitants claimed to have had contact with vaccine baits, whereby most contacts involved children[44]. These contacts do not necessarily lead to true exposure to the vaccine virus. With the hand-out and retrieve system, this kind of direct contact with the vaccine bait is almost completely excluded, although sometimes the owners offer the baits to the dogs. However, indirect human contact with the vaccine virus cannot be excluded as there is a possibility that a dog orally vaccinated will bite or lick someone in the hours following bait consumption. Depending on the vaccine construct used, the viable virus will sometimes remain present in the oral cavity for several hours after bait consumption, and thus the dog can transmit the virus during this period[45]. However, as oral vaccination is targeted at dogs that cannot be restrained and handled without special effort, these animals cannot be marked and are thus not identifiable post-vaccination. Hence, it is difficult to determine the risk of potential human exposure to the vaccine as a result of contact with orally vaccinated dogs. The sachets used in this study contained a blue dye that visibly stained the oral cavity for a period similar to the persistence of viable vaccine virus in the oral cavity after oral vaccination[36]. Hence, during the bait acceptance study and the follow-up survey, it could be estimated that 6.1% of the households providing bait to dogs had direct contact with the dog, as the dye also stains clothes and human skin. All 23 contacts reported were considered Type I according to the WHO categorization for contacts with rabies virus, i.e. touching an animal or licking on intact skin, which is not considered rabies exposures[46]. This underscores the low risk of human exposure to the vaccine-dosed virus using this distribution system. It must be stated here that when using oral rabies vaccines meeting the safety requirements as recommended by WHO and WOAH[39,45], the probability that “true” exposures to the vaccine bait would lead to serious adverse events is negligible, as shown for the 3rd generation oral rabies vaccine, SPBN GASGAS, a candidate for further ORV studies in Bali[41].
CONCLUSIONS
A locally-made intestine bait and an industrially manufactured egg-flavored bait were readily taken up by local dogs in Bali. This ready acceptance of trial baits offers a unique opportunity to deliver effective ORV to dogs that cannot be easily caught and restrained for parenteral vaccination. Most field workers consider ORV to be better suited than CVR for vaccinating these free-roaming dogs. The human risk assessment indicated that in Bali, there is a risk, albeit small, that people can come in contact with the vaccine through direct contact with dogs previously offered a bait. Hence, only vaccines with a high safety profile should be used.
RECOMMENDATION
ORV should replace the presently used method of CVR for free-roaming dogs as a complementary tool to increase vaccination coverage and thus to effectively interrupt rabies transmission among dogs. This will support the elimination of dog-mediated rabies from Bali, and potentially from other areas of Indonesia.
DECLARATIONS
AcknowledgmentsSpecial thanks to Steffen Ortmann (CEVA SA), who prepared the manufacturer’s fishmeal and egg-flavored baits. Appreciation for Denni Rajagukguk and Ni Wayan Wardani (AIHSP), who assisted in the preparation for the local baits and supporting field activities, as well as staff member of Directorate of Animal Health - Ministry of Agriculture, Bali Provincial Animal Health services, Buleleng and Karangasem Districts Animal Health Services for assisting the fieldwork.
Authors’ contributionsDesigned the protocol of the research: Vos A, Husein WF
Prepared and coordinated field activities: Husein WF, Prayoga IMA
Be responsible for data analysis and writing the manuscript: Vos A, Husein WF
All authors were, directly and indirectly, involved in the implementation of field activities.
Availability of data and materialsThe original data can be provided upon reasonable request and should be directed to the corresponding author.
Financial support and sponsorshipThis project was partially funded by the Department of Foreign Affair and Trade (DFAT) of the Australian Government through the Australian Indonesian Health Security Project (AIHSP) and by the United States Agency for International Development (USAID) through the Emergency Center for Transboundary Animal Diseases of the Food and Agriculture Organization of the United Nations (FAO ECTAD) with grant number (G1.2.1131 - OSRO/INS/002/USA).
Conflicts of interestVos A is a full-time employee of a pharmaceutical company manufacturing oral rabies vaccines and baits.
Ethical approval and consent to participateThe study “Assessing Bait Acceptance of Local Dogs, Oral Vaccination Success, and Human Contact Risk in Bali, Indonesia” published in One Health & Implementation Research was approved by the Ethics Committee of the Directorate of Animal Health (No. 16011/PK.350/F4/02/2021).
Consent for publicationWritten informed consent for this study was obtained form all dog owners.
Copyright© The Author(s) 2023.
REFERENCES
1. Susetya H, Sugiyama M, Inagaki A, Ito N, Mudiarto G, Minamoto N. Molecular epidemiology of rabies in Indonesia. Virus Res 2008;135:144-9.
2. Setiawaty V, Septiawati C, Burni E. Karakteristik Kasus fatal Akibat Gigitan hewan penular rabies di Indonesia 2016 - 2017. MPK 2019;29:235-42.
3. Ward MP. Rabies in the Dutch East Indies a century ago - a spatio-temporal case study in disease emergence. Prev Vet Med 2014;114:11-20.
4. Jatikusumah A, Husein WF, Gozali A, et al. Rabies control in indonesia: working together to protect animal and human welfare. In: Stephens T, Editor. One Welfare in Practice. CRC Press, 2021. pp. 179-204.
5. MoA (Ministry of Agriculture), FAO (Food and Agriculture Organization), WAP (World Animal Protection). Masterplan Nasional Pemberantasan Rabies di Indonesia. Available from: https://rr-asia.woah.org/wp-content/uploads/2020/03/roadmap-rabies-v05_indonesia.pdf [Last accessed on 24 Apr 2023].
6. Putra AAG, Hampson K, Girardi J et al. Response to a Rabies Epidemic, Bali, Indonesia, 2008-2011. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647408/pdf/12-0380.pdf [Last accessed on 24 Apr 2023].
7. Haesler B, Gregory N, Bennani H, Gilbert W, Fornace K, Rushton J. Evaluation of Rabies Control in the Province of Bali, Indonesia. Available from: https://drive.google.com/file/d/1QN-m1bD1sN5HZjC8IXRNwTqMoN_HT9nV/view [Last accessed on 25 Apr 2023].
8. Purwo Suseno P, Rysava K, Brum E, et al. Lessons for rabies control and elimination programmes: a decade of One Health experience from Bali, Indonesia. Rev Sci Tech 2019;38:213-24.
9. Sarosa A, Adjid RMA, Syafriati T, Yuningsih. Studi penyakit rabies di daerah endemik: prevalensi infeksi virus rabies pada anjing, kucing dan tikus di kodya padang, sumatera barat. Available from: https://123dok.com/document/y4kolxvq-penyakit-rabies-daerah-endemik-prevalensi-infeksi-padang-sumatera.html [Last accessed on 24 Apr 2023].
10. Cliquet F, Guiot AL, Aubert M, et al. Oral vaccination of dogs: a well-studied and undervalued tool for achieving human and dog rabies elimination. Vet Res 2018;49:1-11.
11. Wallace RM, Cliquet F, Fehlner-Gardiner C, et al. Role of oral rabies vaccines in the elimination of dog-mediated human rabies deaths. Emerg Infect Dis 2020;26:1-9.
12. Darkaoui S, Cliquet F, Wasniewski M, et al. A century spent combating rabies in Morocco (1911-2015): how much longer? Front Vet Sci 2017;4:78.
13. Gibson AD, Yale G, Vos A, et al. Oral bait handout as a method to access roaming dogs for rabies vaccination in Goa, India: a proof of principle study. Vaccine X 2019;1:100015.
14. Estrada R, Vos A, De Leon R, Mueller T. Field trial with oral vaccination of dogs against rabies in the Philippines. BMC Infect Dis 2001;1:23.
15. Undurraga EA, Millien MF, Allel K, et al. Costs and effectiveness of alternative dog vaccination strategies to improve dog population coverage in rural and urban settings during a rabies outbreak. Vaccine 2020;38:6162-73.
16. Mähl P, Cliquet F, Guiot AL, et al. Twenty year experience of the oral rabies vaccine SAG2 in wildlife: a global review. Vet Res 2014;45:1-17.
17. Nani S. Rabies pada anjing di Kabupaten Flores Timur:: studi populasi dan ujicoba oral bait. Available from: http://etd.repository.ugm.ac.id/penelitian/detail/47332# [Last accessed on 24 Apr 2023].
18. Estrada R, Vos A, Rc de L. Acceptability of local made baits for oral vaccination of dogs against rabies in the Philippines. BMC Infect Dis 2001;1:19.
19. Bonwitt J, Bonaparte S, Blanton J, et al. Oral bait preferences and feasibility of oral rabies vaccination in Bangladeshi dogs. Vaccine 2020;38:5021-6.
20. Kasemsuwan S, Chanachai K, Pinyopummintr T, Leelalapongsathon K, Sujit K, Vos A. Field studies evaluating bait acceptance and handling by free-roaming dogs in Thailand. Vet Sci 2018;5:47.
21. Bender S, Bergman D, Vos A, Martin A, Chipman R. Field studies evaluating bait acceptance and handling by dogs in Navajo Nation, USA. Trop Med Infect Dis 2017;2:17.
22. Vos A, Nokireki T, Isomursu M, et al. Oral vaccination of foxes and raccoon dogs against rabies with the 3rd generation oral rabies virus vaccine, SPBN GASGAS, in Finland. Acta Vet Scand 2021;63:1-8.
23. Cliquet F, Barrat J, Guiot AL, et al. Efficacy and bait acceptance of vaccinia vectored rabies glycoprotein vaccine in captive foxes (Vulpes vulpes), raccoon dogs (Nyctereutes procyonoides) and dogs (Canis familiaris). Vaccine 2008;26:4627-38.
24. Olsevskis E, Liepins E, Lamberga K, Rodze I. Efficacy of the first large-scale rabies oral vaccination campaigns in Latvia. Available from: https://agris.fao.org/agris-search/search.do?recordID=LV2012000047 [Last accessed on 24 Apr 2023].
25. Kharmachi H, Haddad N, Matter H. Tests of four baits for oral vaccination of dogs against rabies in Tunisia. Vet Rec 1992;130:494.
26. Linhart SB, Baer GM, Balderas Torres JM, et al. Acceptance of candidate baits by domestic dogs for delivery of oral rabies vaccines. Onderstepoort J Vet Res 1997;64:115-24.
27. Gibson AD, Mazeri S, Yale G, et al. Development of a non-meat-based, mass producible and effective bait for oral vaccination of dogs against rabies in Goa State, India. Trop Med Infect Dis 2019;4:118.
28. Schuster P, Gülsen N, Neubert A, Vos A. Field trials evaluating bait uptake by an urban dog population in Turkey. Available from: https://drive.google.com/file/d/1ou_RARD344C4Iybmd1fRkewsUtchmjCB/view [Last accessed on 25 Apr 2023].
29. Frontini MG, Fishbein DB, Garza Ramos J, et al. A field evaluation in Mexico of four baits for oral rabies vaccination of dogs. Am J Trop Med Hyg 1992;47:310-6.
30. Matter HC, Kharmachi H, Haddad N, et al. Test of three bait types for oral immunization of dogs against rabies in Tunisia. Am J Trop Med Hyg 1995;52:489-95.
31. Berentsen AR, Bender S, Bender P, et al. Preference among 7 bait flavors delivered to domestic dogs in Arizona: implications for oral rabies vaccination on the Navajo Nation. J Vet Behav 2014;9:169-71.
32. Corn JL, Méndez JR, Catalán EE. Evaluation of baits for delivery of oral rabies vaccine to dogs in guatemala. Am J Trop Med Hyg 2003;69:155-8.
33. Smith TG, Millien M, Vos A, et al. Evaluation of immune responses in dogs to oral rabies vaccine under field conditions. Vaccine 2019;37:4743-9.
34. Chanachai K, Wongphruksasoong V, Vos A, et al. Feasibility and effectiveness studies with oral vaccination of free-roaming dogs against rabies in Thailand. Viruses 2021;13:571.
35. Te Kamp V, Freuling C M, Vos A, et al. Oral rabies vaccination of wildlife: what drives vaccine uptake efficiency in different reservoir species. Sci Rep 2020;10:2919.
36. Langguth A, Leelahapongsathon K, Wannapong N, et al. Comparative study of optical markers to assess bait system efficiency concerning vaccine release in the oral cavity of dogs. Viruses 2021;13:1382.
37. Molini U, Hassel R, Ortmann S, et al. Immunogenicity of the oral rabies vaccine strain SPBN GASGAS in dogs under field settings in Namibia. Front Vet Sci 2021;8:737250.
38. Leelahapongsathon K, Kasemsuwan S, Pinyopummintr T, et al. Humoral immune response of thai dogs after oral vaccination against rabies with the SPBN GASGAS vaccine strain. Vaccines 2020;8:573.
39. Güzel N, Leloglu N, Vos A. Evaluation of a vaccination campaign of dogs against rabies, including oral vaccination in Kusadasi, Turkey. Available from: https://dergipark.org.tr/en/download/article-file/2252984 [Last accessed on 24 Apr 2023].
40. OIE (World Organisation for Animal Health). Manual of Diagnostic Tests and Vaccines for Terrestrial Animals 2018; OIE: Paris, France, 2018, Chapter 3.1.17. Available from: https://www.woah.org/en/produit/manual-of-diagnostic-tests-and-vaccines-for-terrestrial-animals-2018/ [Last accessed on 24 Apr 2023].
41. Head JR, Vos A, Blanton J, et al. Environmental distribution of certain modified live-virus vaccines with a high safety profile presents a low-risk, high-reward to control zoonotic diseases. Sci Rep 2019;9:6783.
42. Vos A. Oral vaccination of dogs against rabies. Available from: https://drive.google.com/file/d/1EUcWPI5-vFKSUiIHzHwJGTo4Ejn8egxb/view [Last accessed on 25 Apr 2023].
43. Matter HC, Schumacher CL, Kharmachi H, et al. Field evaluation of two bait delivery systems for the oral immunization of dogs against rabies in Tunisia. Vaccine 1998;16:657-65.
44. Ben Youssef S, Matter HC, Schumacher CL, et al. Field evaluation of a dog owner, participation-based, bait delivery system for the oral immunization of dogs against rabies in Tunisia. Am J Trop Med Hyg 1998;58:835-45.
45. Vos A, Freuling C, Ortmann S, et al. An assessment of shedding with the oral rabies virus vaccine strain SPBN GASGAS in target and non-target species. Vaccine 2018;36:811-7.
46. World Health Organization (WHO). WHO expert consultation on rabies: third report. World Health Organization; 2018.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Husein WF, Saputra ILM, Suseno PP, Arthawan IM, Prayoga IMA, Daryono J, Vos A, Wicaksono A, Schoonman L, Weaver J, Zainuddin N. Assessing bait acceptance of local dogs, oral rabies vaccination success and human contact risk in Bali, Indonesia. One Health Implement Res 2023;3:16-29. http://dx.doi.org/10.20517/ohir.2022.32
AMA Style
Husein WF, Saputra ILM, Suseno PP, Arthawan IM, Prayoga IMA, Daryono J, Vos A, Wicaksono A, Schoonman L, Weaver J, Zainuddin N. Assessing bait acceptance of local dogs, oral rabies vaccination success and human contact risk in Bali, Indonesia. One Health & Implementation Research. 2023; 3(2): 16-29. http://dx.doi.org/10.20517/ohir.2022.32
Chicago/Turabian Style
Husein, Wahid Fakhri, Irene Linda Megawati Saputra, Pebi Purwo Suseno, I Made Arthawan, I Made Angga Prayoga, Joko Daryono, Ad Vos, Arief Wicaksono, Luuk Schoonman, John Weaver, Nuryani Zainuddin. 2023. "Assessing bait acceptance of local dogs, oral rabies vaccination success and human contact risk in Bali, Indonesia" One Health & Implementation Research. 3, no.2: 16-29. http://dx.doi.org/10.20517/ohir.2022.32
ACS Style
Husein, WF.; Saputra ILM.; Suseno PP.; Arthawan IM.; Prayoga IMA.; Daryono J.; Vos A.; Wicaksono A.; Schoonman L.; Weaver J.; Zainuddin N. Assessing bait acceptance of local dogs, oral rabies vaccination success and human contact risk in Bali, Indonesia. One. Health Implement. Res. 2023, 3, 16-29. http://dx.doi.org/10.20517/ohir.2022.32
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 15 clicks
Cite This Article 15 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.