Onchocercal skin disease in Benue state, Nigeria: integrated assessment of burden and psychosocial impact, and associated factors
Abstract
Aim: We aimed to measure the degree to which onchocercal skin disease (OSD) impairs quality of life (QoL) in endemic resource-poor communities in the Ushongo, Kwande, and Katsina-ale local government areas of Benue State, Nigeria.
Methods: We evaluated the skin characteristics and QoL of 307 children and adults with OSD using a modified dermatological life quality index (mDLQI). Assessment of OSD was conducted and scored using mDLQI from 0 (no effects) to 18 (large effects). Thereafter, structured questionnaires were applied to assess the knowledge, attitudes, and predictors of moderate and severe OSD patients.
Results: In total, 235/307 (76.5%) participants presented onchocercal nodules; chronic papular dermatitis was found in 68 (22.1%). A total of 288 (93.8%) had two or more OSD-associated symptoms. The median mDLQI score was 0 [interquartile range (IQR): 0-0] in children and 5 in adults (IQR: 2-8). A higher mDLQI median score was observed in farmers. There was a statistically significant difference between children and adults (P < 0.001). The most frequently reported impairments were social exclusion, embarrassment/shame, and restriction from work/leisure activities. In logistic regression analysis, there was a significant association with increasing age (adjusted odds ratio (AOR) = 1.44; 95%CI: 1.21-1.71; P < 0.001) and visual impairment (AOR = 1.78; 95%CI: 1.02-3.10; P = 0.040) with severe mDLQI. Papular rash was an independent protective factor (AOR = 0.50; 95%CI: 0.27-0.93; P = 0.030).
Conclusion: Onchocerciasis-related morbidity has a profound measurable impact on the individual QoL, affecting the overall socioeconomic well-being of the affected community, if left untreated. Therefore, strict supervision and follow-up of home-based mass treatment with ivermectin are vital for successful control of the disease and to reduce the burden on affected communities.
Keywords
INTRODUCTION
Onchocerciasis (river blindness) has caused profound morbidity and mortality in endemic areas, mainly in Sub-Saharan Africa, with over 120 million people living in endemic areas worldwide[1-3]. The burden of onchocerciasis in severely affected populations in Sub-Saharan Africa is marked by various types of skin and eye diseases that lead to considerable negative social and economic effects such as low self-esteem, ostracization, decreased productivity, and suicide attempts[4-6]. Despite considerable success in the control of onchocerciasis during the last decades, irreversible blindness and elephantiasis of the scrotum are not uncommon in adults in many endemic communities.
About 12.2 million people suffer from onchocercal skin disease (OSD). The disease is characterized by infection associated with subcutaneous nodules, severe itching, and dermatological changes, such as depigmentation, lichenification, and atrophy[2,4]. Social stigma such as discriminatory response, avoidance, and ostracism lead to loss of self-confidence, poverty as productivity decreases, and reduced life expectancy by up to 15 years[7,8]. The physical and psychosocial impacts of the infection are profound, as the educational chances of children who become carers of disabled adults are abridged[9,10]. The degree of clinical pathology varies with geographical locations, parasite strain, and environmental and human host factors[11]. The stigma and discrimination associated with onchocerciasis are closely related to the severity of OSD that significantly affects the quality of life as a consequence of the depressive symptom and social isolation of the affected[4,8,9,12].
Nigeria has been ranked as the most onchocerciasis-endemic country in Sub-Saharan Africa, with about seven million prevalent cases (about 40% of global cases)[2,7,13]. The country initiated a national control program with support from WHO/APOC in 1995, based on a regular mass drug administration (MDA) of ivermectin[14]. Ivermectin is a safe and potent broad-spectrum anthelminthic drug that successfully reduces infection and transmission with few adverse events[15]. The overall objective addresses the WHO sustainable Millennium Development Goals (MDGs) of improving health, reducing illiteracy and poverty, and promoting economic development in endemic communities. The success of periodic MDA depends on the duration of the treatment program, anchored on spatial epidemiological data, including the parasite strain, clinical picture, knowledge, cultural beliefs, and practices of individuals[16,17]. Several studies have revealed the public health importance of nodules and OSD, but there is a lack of reliable diagnostic tools for the surveillance and monitoring of the disease in high-risk areas[4,18,19]. Only a few validated standard methods have been used to qualitatively evaluate the quality of life (QoL) of patients with OSD[4,20,21]. Studies on the psychosocial and socioeconomic consequences of the disease on the affected populations in Nigeria have been well documented[4,9,21,22]. However, to follow an integrated control concept based on One Health principles, additional information on the degree of disability caused by onchocerciasis is needed. In this study, to measure the degree to which onchocercal skin disease (OSD) impairs QoL in endemic resource-poor communities in Benue State, Nigeria, we assessed the prevalence, burden, and socioenvironmental variables associated with onchocerciasis in endemic communities and applied the modified dermatological quality of life index (iDLQI) to measure the QoL of OSD patients. Factors associated with a considerable impact on QoL were assessed.
METHODS
Study area
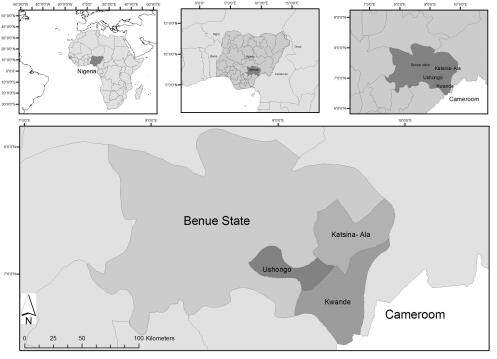
We conducted the study in four onchocerciasis hyper-endemic communities in three contiguous local government areas (LGAs) in the east of Benue State, Nigeria (7°20′ N 8°45′ E), namely Ushongo, Kwande, and Katsina-Ale [Figure 1]. A household census conducted in the study area before data collection identified a total of 1593 households (about 11,948 individuals). The communities were considered as one study area for this study.
Detailed geography and characteristics of the study area have been previously described[23]. In brief, the communities are located along the tributaries of River Benue at an elevation of about 380 m. The area is characterized by tropical guinea savannah vegetation with an average daily temperature of 35-37°C during the hot-dry season (November to April) and a mean annual precipitation range of 1200-1800 mm in the wet months (May to October).
The residents are primarily subsistence farmers of food crops, majorly of Idoma and Tiv ethnic groups, and of Christian faith. Illiteracy rates are high. There is a water project for the inhabitants, but small rivers, streams, and dug wells serve as sources of water supply for domestic consumption and farming purpose. About 85% of the households have a monthly per capita income of < N 18,000 (the equivalent of US $50 at the time of the study), the national minimum wage. Hygienic conditions are precarious, as waste and garbage are scattered indiscriminately around houses, and there is no public waste collection. Periodic MDA with ivermectin for the control of onchocerciasis was launched by WHO in the area in the early 2000s, with the installation of rural healthcare centers for the treatment of patients. If necessary, patients are referred to specialized hospitals in Makurdi, the state capital.
Study population and design
Prior to the study, the research protocol was reviewed by the ethical committee of the Faculty of Life Sciences, University of Ilorin, the administrative authorities of the Benue State Ministry of Health, and community leaders. Informed consent was obtained from every individual including the legal caregivers of the minor after a detailed explanation of the study protocol.
A cross-sectional study was conducted after the screening, assessment of skin microfilarial load, and ivermectin treatment by health authorities who also provided information on the infection status and treatment of all inhabitants in the communities.
All inhabitants of the communities who had spent at least 5 years in the community, with a history of > 12 months of ivermectin treatment, and 9 years of age were eligible. Individuals who declined participation and/or with contraindication to ivermectin treatment were not included. Considering non-participation and cluster effects, 212 households consisting of 1590 individuals were selected randomly, using a random numbers generator (Epi Info Software package, version 6.04d).
Households were visited and individuals were interviewed to obtain information on demographic data (such as name, gender, marital status, and educational status) and socioeconomic factors (such as occupation, monthly income, house structure, and household characteristics). In addition, knowledge of onchocerciasis and its transmission and treatment was assessed. The epidemiological characteristics and psychosocial impact of onchocerciasis were assessed using the semi-quantitative modified disability life quality index (mDLQI) questionnaires[24].
Thereafter, the skin of each participant was thoroughly examined by two investigators of Benue State origin, who have been involved in the onchocerciasis studies in the state (AB, a postgraduate student in the Parasitology Unit at the Department of Zoology and NA, a researcher and senior academic staff at the College of Medicine), using non-invasive rapid assessment method[25]. The entire body was carefully examined in a well-lighted room where privacy was guaranteed. OSD signs diagnostic for onchocerciasis (papular dermatitis, skin lichenification, palpable nodules, dermal atrophy, depigmentation, and hanging groin) were clinically assessed and classified as described by Murdoch et al.[26]. To reduce observation bias, skin examination and interviews were conducted by different persons, and the interviewer was blinded regarding the clinical examination.
Additional differential diagnosis was not conducted since the local authority health teams had, prior to the study, screened the study population (by skin snip examination - the gold standard) for microfilarial load, identified positive cases, and commenced treatment. Data collection was concluded before the onset of the COVID-19 pandemic.
Modified dermatology life quality index (mDLQI)
The mDLQI questionnaire created by Worth et al., which was originally elaborated for scabies, was adapted to the onchocerciasis setting[24]. The questions focus on clinical sequels of onchocerciasis and the psychosocial impact OSD may have on affected individuals. The questionnaires were translated and administered in the local language to both adults and children. In accordance with the original version for children, questions on the impact of onchocerciasis on sexual life were changed[24]. The questionnaires were translated into the local Tiv and Idoma languages and pretested in a standardized manner before they were administered to the study participants. Responses were categorized into an ordinal scale of not at all (0), only a little (1), quite a lot (2), and very much (3), giving a total maximum score of 18 (6 questions). The effect of OSD on individuals’ lives was derived from mDLQI scores: none (scores 0-1), small (2-5), moderate (6-10), and large (11-18).
Statistical analysis
Data were double entered, merged into a single dataset, and checked for accuracy. Analysis was done using the Stata software version 15.1 (StataCorp, College Station, TX, USA). Descriptive statistics were tabulated, and the independent variables were analyzed in a bivariate manner to determine the relationship of OSD with quality of life. We re-categorized the mDLQI score into a binary variable, with a positive outcome defined as a moderate or large effect (mDLQI scores 6-18).
The variables that presented statistical significance with a P-value ≤ 0.25 were selected for the multivariate analysis. Logistic regression was performed to estimate the adjusted odds ratios and their confidence intervals. We applied a hierarchical model, first including the age group in the model, and then including one variable of each block at a time. Aside from the age groups retained in the final model, none of the sociodemographic variables remained important.
RESULTS
Of the target population of 1590 individuals (885 males and 705 females) belonging to 212 households, 1323 (83.2%) fulfilled the inclusion criteria. Of these, 307 (23.2%) participated in the study, while 548 declined participation for lack of monetary/material incentive, 435 abstained for cultural reasons, and 33 were not encountered after repeated visits.
The demographical and clinical characteristics of the study population are depicted in Table 1. The median age was 40 years, and about 62% were males, residing in the communities of Saati-Agirigi (63), Saatikyo (67), Manyam (125), and Hitom (52). The median time living in the communities was 28 years (IQR: 5-45 years). Overall, 94% had at least two onchocerciasis-associated symptoms. Onchocercal nodules were the most common manifestation of positive individuals, followed by chronic popular dermatitis and secondary skin infections [Table 1]. Almost 25% of the individuals presented papular dermatitis. Atrophy, hanging groin, hernia, and hydrocele were less common. Severe morbidity of more than five nodules per patient was observed in 4.5% of the affected population [Table 1].
Demographic and clinical characteristics of the study population (n = 307)
| Variables | Numbers |
| Age in years: median (range/IQR) | 40 (3-100/25-55) |
| No. of males/females | 189 (61.6%)/118(38.4%) |
| Age of males: median (range/IQR) | 45 (3-100/29-55) |
| Age of females: median (range/IQR) | 35 (9-90/20-50) |
| Duration in years in community: median (range/IQR) | 28(1-100/15-45) |
| Educational level: | N (%) |
| Illiterate | 89 (29.0%) |
| Primary | 108 (35.2%) |
| Secondary/tertiary | 110 (35.8%) |
| Onchocerciasis-associated signs and symptoms | N (%) |
| Nodules | 235 (76.5) |
| Chronic papular dermatitis | 68 (22.1) |
| Secondary skin infections* | 83 (27.0) |
| Depigmentation (leopard skin) | 59 (19.2) |
| Acute papular dermatitis | 68(14.3) |
| Lichenified dermatitis | 6 (1.3) |
| Hanging groin | 3 (1.0) |
| Hernia | 4 (1.3) |
| Hydrocele | 3 (1.0) |
| Atrophy | 13 (4.2) |
| Two symptoms or more | 288 (93.8) |
| N0. of nodules/patient: median (range/IQR) | 2.0 (1-13/1-3) |
| 0 nodules | 72 (23.4) |
| 1-4 nodules | 220 (71.6) |
| 5-9 nodules | 9 (2.9) |
| 10 or more nodules | 5 (1.6) |
The impairment of quality of life in both adults and children is presented in Figure 2. The median score was 0 [interquartile range (IQR): 0-0] in children and 5 (IQR: 2-8; P < 0.001) in adults. Comparatively, the frequency of mDLQI in adults and children shows that work activities are most commonly affected by OSD. Feeling embarrassed/ashamed and social exclusion were more commonly reported in adults than children. Quality of life in the dressing activities was less commonly reported by both children and adults [Figure 2].
Figure 2. Frequency of dermatology life quality index (DLQI) dimensions in adults (A) and children (B) in Benue State, Nigeria.
The bivariate analysis identified older age and marital status as associated factors with moderate or large effects [Table 2]. The mDLQI was higher in farmers and males. Apart from visual impairment, unpleasant skin conditions, such as itching, excoriation, itching, secondary infection, nodules, and leopard skin, were associated with a moderate or large effect on the quality of life [Table 3]. In logistic regression analysis, there was a significant association between increasing age (adjusted odds ratio = 1.44; 95%CI: 1.21-1.71; P < 0.001) with a severe mDLQI score. Visual impairment remained significantly associated with severe mDLQI (adjusted odds ratio = 1.78; 95%CI: 1.02-3.10; P = 0.040). The presence of papular rash was an independent protective factor for mDLQI severity (adjusted odds ratio = 0.50; 95%CI: 0.27-0.93; P = 0.030).
Sociodemographic variables associated with the moderate or very high effect of onchocerciasis in the mDLQI scale in Benue State, Nigeria
| Variables | Total | mDLQI - moderate or very high effect | P-value | |||
| N | % | RR | 95%CI | |||
| Age group (years) | ||||||
| 0-20 | 48 | 3 | 6.2 | 1 | - | < 0.001 |
| 20-39 | 92 | 40 | 43.5 | 6.95 | 2.26-21.32 | |
| 40-60 | 103 | 49 | 47.6 | 7.61 | 2.49-23.19 | |
| > 60 | 64 | 33 | 51.5 | 8.25 | 2.68-25.31 | |
| Sex | ||||||
| Female | 118 | 40 | 33.9 | 1 | - | 0.055 |
| Male | 189 | 85 | 45.0 | 1.32 | 0.98-1.78 | |
| Marital status | ||||||
| Single/divorced | 61 | 13 | 21.3 | 1 | - | < 0.001 |
| Married | 246 | 112 | 45.5 | 2.13 | 1.29-3.52 | |
| Illiteracy | 89 | 37 | 41.6 | 1.24 | 0.76-1.38 | 0.845 |
| Farmer | 238 | 104 | 43.7 | 1.37 | 0.93-2.01 | 0.083 |
| Monthly income of family head | ||||||
| < n (15,000) n (15,000-30,000) > n (30,000) | 180 71 56 | 72 31 22 | 40.0 43.7 39.3 | 1 1.09 0.98 | - 0.79-1.50 0.67-1.42 | 0.843 |
| House type | ||||||
| Bricks Palm/vegetal | 95 212 | 45 80 | 47.4 37.7 | 1 0.79 | - 0.60-1.04 | 0.112 |
| House light | 20 | 10 | 50.0 | 0.80 | 0.50-1.27 | 0.382 |
| Waste disposal site | ||||||
| Far from house Close to house | 43 263 | 17 107 | 40.7 39.5 | 1 1.03 | - 0.69-1.53 | 0.887 |
| Use open tanks as water storage system | 125 | 117 | 50.0 | 0.80 | 0.48-1.34 | 0.437 |
| Walking distance from house to river | ||||||
| > 10 minutes < 10 minutes | 169 136 | 62 63 | 36.7 45.6 | 1 1.24 | - 0.94-1.62 | 0.116 |
| Community | ||||||
| Saati-Agirigi Saatikyo Manyam Hitom | 63 67 125 52 | 30 26 51 18 | 47.6 38.8 47.6 34.6 | 1 0.81 0.85 0.72 | - 0.54-1.21 0.61-1.19 0.46-1.14 | 0.542 |
Symptoms and treatment associated with the moderate or very high effect of onchocerciasis in the mDLQI scale in Benue State, Nigeria
| Symptoms variables | Total | mDLQI - Moderate or very high effect | P-value | |||
| N | % | RR | 95%CI | |||
| Itching Degree of itching (n = 182) | 192 | 83 | 43.2 | 1.18 | 0.88-1.58 | 0.247 |
| Light | 35 | 16 | 51.4 | 1 | - | 0.319 |
| Moderate | 65 | 24 | 36.9 | 0.72 | 0.45-1.13 | |
| Severe | 82 | 38 | 46.3 | 0.90 | 0.60-1.34 | |
| Excoriation Degree of excoriation (n = 155) | 162 | 71 | 43.8 | 1.17 | 0.89-1.54 | 0.241 |
| < 3 tracks | 32 | 12 | 37.5 | 1 | - | 0.522 |
| 3-5 tracks | 80 | 37 | 46.2 | 1.23 | 0.74-2.04 | |
| 6-10 tracks | 39 | 18 | 46.1 | 1.23 | 0.70-2.15 | |
| > 10 tracks | 4 | 3 | 75.0 | 2.00 | 0.97-4.11 | |
| Secondary infection | 83 | 38 | 45.8 | 1.17 | 0.88-1.56 | 0.271 |
| Leopard skin | 59 | 26 | 44.1 | 1.10 | 0.79-1.52 | 0.560 |
| Papular rash | 68 | 19 | 27.9 | 0.62 | 0.42-0.94 | 0.015 |
| Lizard/Crocodile skin | 6 | 3 | 50.0 | 1.23 | 0.54-2.77 | 0.640 |
| Hanging groin | 3 | 1 | 33.3 | 0.81 | 0.16-4.07 | 0.794 |
| Hernia | 4 | 3 | 75.0 | 1.86 | 1.04-3.33 | 0.308* |
| Hydrocele | 3 | 2 | 66.7 | 1.64 | 0.73-3.71 | 0.569* |
| Presence of nodules | 235 | 101 | 43.0 | 1.29 | 0.90-1.84 | 0.145 |
| Atrophy | 13 | 5 | 38.4 | 0.94 | 0.46-1.89 | 0.866 |
| Visually impaired | 203 | 97 | 47.8 | 1.77 | 1.25-2.51 | < 0.001 |
| Treatment | ||||||
| Infection status | 304 | 125 | 41.1 | - | - | 0.149 |
| Currently on drugs | 269 | 110 | 33.0 | 1.03 | 0.68-1.57 | 0.868 |
Table 4 shows that knowledge of the disease was significantly associated with a moderate or high effect of onchocerciasis on the mDLQI scale. Comparatively, the mode of treatment and level of compliance to treatment had a higher median mDLQI score than treatment of the disease during infection.
Knowledge associated with the moderate or very high effect of onchocerciasis in the mDLQI scale in Benue State, Nigeria
| Knowledge variables | Total | mDLQI - Moderate or very high effect | P-value | |||
| N | % | RR | 95%CI | |||
| Heard of the disease before | 294 | 125 | 42,5 | - | - | 0.002* |
| Knowledge of transmission by insect bite | 229 | 95 | 41.5 | 1.07 | 0.78-1.48 | 0.639 |
| Belief in being caused by a spiritual problem | 1 | 0 | 0.0 | 0 | - | 1.000* |
| Belief of transmission by drinking or taking a bath in the river | 30 | 12 | 40.0 | 0.98 | 0.61-1.55 | 0.933 |
| Treatment during infection | 269 | 110 | 33.0 | 1.03 | 0.68-1.57 | 0.868 |
| Knowledge of the method of treatment | ||||||
| Drugs | 264 | 108 | 40.9 | 1 | - | 0.453* |
| Herbal | 7 | 4 | 57.1 | 1.40 | 0.72-2.69 | |
| Level of compliance with MDA | ||||||
| No compliance | 25 | 11 | 44.0 | 1 | - | 0.673 |
| Half compliance | 79 | 29 | 36.7 | 0.83 | 0.49-1.41 | |
| Full compliance | 161 | 68 | 42.2 | 1.34 | 0.59-1.55 | |
DISCUSSION
In this study, we found for the first time that OSD affects the QoL of both children and adults in Nigeria. We adapted DLQI, a self-explanatory questionnaire, confirmed to be most suitable for assessing different skin diseases[24]. The mDLQI score correlated with the severity of OSD. The outcome strengthens previously reported data on the negative impacts of OSD on the QoL from similar endemic areas in tropical Africa.
Nearly all common clinical signs and symptoms associated with onchocerciasis were reported, indicating the endemicity of infection in the area. While this is consistent with the previously reported data from the same geographical zone[22,23,27], the prevalence of OSD was comparatively lower in this study. About 30% of the population with moderate and heavy OSD reported a negative impact on their QoL, with a median mDLQI score of 4, suggesting a downward change from the burden of the negative impacts of the disease, possibly due to the effectiveness of the ongoing control program with ivermectin. However, a significant proportion of the study population presented palpable nodules, the most realistic diagnostic sign, and OSD, commonly pruritus, papular onchocercal dermatitis, atrophy, and depigmentation, as reported in many onchocerciasis-endemic areas in Nigeria and other west African countries[15,28,29]. This underscores either the irreversibility of chronic skin pathologies due to onchocerciasis or a subsisting low-grade transmission.
The mDLQI scores were determined by the dermal form of the disease known to have tremendous psychosocial effects on the patient due to color and texture changes of the skin[25]. Remme[30] observed that the burden of OSD alone was greater than the burden of visual impairment and blindness. Onchocercal pruritus often marks onchocercal infection and causes severe itching and scratching that leads to sleeplessness, fatigue, general debilitation, and harmful psychosocial effects[5,9,29]. In Nigeria, incessant itchy skin results in excoriation and subsequent superinfection with bacteria that affects women to insufficiently breastfeed their infants[5,29]. Surprisingly, qualitative information on the effects of itching and reactive skin lesions on the quality of life of the affected population is limited in many endemic populations in Nigeria. Quality of life is a multidimensional entity that can only be measured when the relevant facets are evaluated[24]. In this study, we modified and adapted DLQI to the local culture, an explanatory questionnaire that satisfactorily evaluates the pathophysiological and psychological features of OSD on the QoL in adults and children. Consistent with the reports on the association of onchocerciasis infection with age[4,16,29,31], our findings on the perception of the degree of impairment are clearly age-dependent, relative to the difference in the occurrence and severity of skin disease between adults and children in the first two decades of age.
In this study, problems faced at work and schools were generally the most frequent cause of QoL impairment in adults and children. This portends a grave socioeconomic consequence because onchocerciasis is an occupational disease of peasant farmers, unskilled laborers, and nomads and fishermen involved in outdoor activities. In endemic areas in southwestern Nigeria, Oladipo et al. observed that farmers with severe OSD had less farmland for cultivation[32]. This may induce low agricultural and economic productivities, which may lead to decreased earnings rates and increased financial strains - a condition with a high risk of developing depression[12]. In children, absenteeism from school due to stigmatization leads to high school dropout. Brieger et al. reported that children in western Nigeria dropped out of school as a consequence of OSD[9]. This is usually three-fold higher in households with severe OSD than in households without OSD[2]. All of these may threaten the occupational and economic opportunities in the endemic population. Paradoxically, many long-term residents living in impoverished settings with extreme poverty perceive onchocerciasis-induced misery as a negligible health issue compared to daily life problems.
Other emotional aspects also reported by respondents were that discomfort and restriction on leisure and sexual activities regarding their imperfect body image. These impacts of stigma were reported more by adult than child respondents. This reflects the age-dependent burden of OSD observed in Africa[4,28]. The perception of adults with regard to sexual relationships may be gender related. Although severe OSD is not sexually transmitted, the unpleasant appearance of ulcerative genital lesions and lichenified and depigmented skin considerably lower self-esteem and cause frustration, depression, and marital problems. Especially young single women, being more concerned about their appearance, feel the brunt of sexual unattractiveness compared to men, because it may affect the prospect of marriage. Yew et al. showed that adult atopic dermatitis was significantly associated with a high rate of divorce and separation in the United States[12]. This study also showed that most variability in the severity of OSD is significantly associated with differences in age, marital status, and socioeconomic factors such as occupation and income.
Peasant farmers had high mDLQI scores. This can be ascribed to the ecological and behavioral factors that favor intense parasite/vectors contacts. Earlier reports[33,34] showed that the biting behavior of the blackfly vector Simulium damnosum and the peak of parasite transmission occur during the dry-hot season (January to May), which coincides with the critical period of clearing and planting season for farmers in the study area. The work activities induce full or partial exposure of the body, thus increasing vector contact.
Our observation on the association of poor knowledge of disease transmission and use of herbal treatment on mDLQI score was substantial for concern. Although much of the population had appreciable knowledge about onchocerciasis, the knowledge gap on disease transmission, diagnosis, and treatment was extensive. This portends serious public health challenges when infected residents of endemic areas migrate to non-endemic areas with similar ecological conditions.
Anecdotal evidence confirms that onchocercal itching is ascribed to the bite of insects, possibly blackfly vector or midges. Domche et al. reported that the duration of residency and age of individuals in endemic communities were associated with good knowledge and perception of the disease[35]. However, poor knowledge of the disease can be attributed to poor education by the community mobilization and sensitization teams. The consequences of this on the entire community and control measures are grave, considering that ignorance of disease transmission increases exposure to infection. Our study population was predominantly of low income and low level of education. These features are proxies for poor living conditions and personal and environmental hygiene. Individuals with poor living conditions where adequate and affordable healthcare services are inaccessible would seek alternative treatment to ameliorate the burden of infection. It is, therefore, not a surprise that participants would prefer herbal treatment, and it partly explains why reported cases of onchocerciasis-associated epilepsy and nodding syndrome in infected poor individuals in rural settings are common.
Onchocerciasis is a disfiguring arthropod-borne parasitic disease that is inextricably linked with other neglected tropical diseases that form part of the vicious cycle of poverty in many endemic areas in Africa. The control program by MDAs meets the WHO sustainable development goals that aim to reduce illiteracy and extreme poverty, ensure equity, and improve the health and well-being of individuals as well as the economic development of the affected populations. Under the Africa Programme for Onchocerciasis Control (APOC) mandate, MDA of ivermectin to the target populations remains the only “vertical” control approach to impede disease transmission and improve people’s quality of life and personal health. In many endemic rural communities in Nigeria, where gastrointestinal helminthiasis, schistosomiasis, strongyloidiasis, loiasis, and malaria coexist with the targeted onchocerciasis[36], helminthic diseases such as strongyloidiasis, filariasis, and cestodiasis are susceptible to ivermectin treatment. The One Health approach of integrating the onchocerciasis vertical control program with existing WHO programs will not only enhance efficient drug delivery but also stimulate commitment, sustainability, and cost-effectiveness. Furthermore, ivermectin is a broad-spectrum antiparasitic drug for a wide range of human skin-borne parasitic arthropods such as scabies, cutaneous larva migrans, pediculosis, and myiasis[37]; the intervention with ivermectin would effectively and safely reduce the occurrence of other parasitic infections. Our findings also provide evidence of the need to incorporate QoL of the affected population in post-intervention surveillance that detects recrudescence and resistance of infection. It is believed that elimination of onchocerciasis is achievable when treatment of target areas is simultaneously maintained with blackfly vector (Simulium damnosum) control through a larvicidal approach and environmental changes. This cross-linkage of disease control programs would, by extension, ameliorate the nuisance and transmission of other water-borne vectors of species of Plasmodium, Wuchereria, Leishmania, and Loa.
There are several limitations to this study. First, the samples were localized in three selected endemic communities within a state of Nigeria, with many households not participating due to specific local cultural practices and other constraints, and participation rates were low. Therefore, the generalizability of the results may be limited, and there may be an underrepresentation of individuals with skin disease. There may also have been a gender participation bias, as women may have declined skin examination for cultural reasons more often than men or did not feel eligible to be pregnant/caring for babies. Women may also have been treated with ivermectin more regularly than men in the past, and there may have been fewer women fulfilling the criterion of having been treated for more than 12 months. Given that most of the respondents were already on active ivermectin treatment, this ameliorated the disease condition and may have led to an underestimation of the negative social effects of the disease. Secondly, the awareness of observers in endemic areas could possibly create observer bias, particularly when microfilaria load of the sampled populations was not determined for confirmation of infection. Despite these limitations, we believe that the study significantly contributes to knowledge on the topic in Nigeria and provides information for the elaboration of control measures within a One Health approach, also considering psychosocial effects of the disease.
In conclusion, this study provides evidence for the need for constant re-evaluation of onchocerciasis status in many endemic areas in Africa. The psychosocial impact of OSD has to be considered when planning and conducting control measures. An evaluation that considers the different requirements of various pathological groups will further improve the control program. Additional universal metrics could be used in future studies to describe the burden of disease, such as disability-adjusted life years.
Disclaimer
This study on the psychosocial impact of onchocerciasis and associated risk factors does not require any drug administration on the disease-affected population in the study area. However, references were made about the use of ivermectin drug to keep our information up to date. The expressed or implied opinions about the reliability and/or suitability of the drug are solely that of the authors, who make no warranties or representation of any kind.
DECLARATIONS
Authors’ contributions
Designed the study and wrote the draft: Ugbomoiko SU, Heukelbach J
Recruited the patients: Bem A and Amase N
Fieldwork: Bem A, Babamale AO, Adegbola RQ, Amase N, Ugbomoiko SU, supported by a nurse and technician
Analyzed the data: Heukelbach J and Alencar CH
All authors added their contributions and comments and approved the final version of the manuscript.
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
This study was approved by the Benue State Ministry of Health and the University of Ilorin ethical review Boards after a detailed explanation of the study's objectives and protocol. Community leaders also approved the study. Prior to the study, participants signed the locally translated informed consent forms and confidentiality was maintained for the data obtained from patients. The legal caregiver of children gave informed consent to enrol a child.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2022.
REFERENCES
1. Brattig NW. Successful elimination of onchocerciasis (river blindness) vectors from isolated foci in two African countries. Acta Trop 2009;111:201-2.
2. Hotez PJ, Kamath A. Neglected tropical diseases in sub-saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Negl Trop Dis 2009;3:e412.
3. Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet 2017;390:1211-59.
4. Murdoch ME, Asuzu MC, Hagan M, et al. Onchocerciasis: the clinical and epidemiological burden of skin disease in Africa. Ann Trop Med Parasitol 2002;96:283-96.
5. Amazigo OU. Detrimental effects of onchocerciasis on marriage age and breast-feeding. Trop Geogr Med 1994;46:322-5.
6. Vinkeles Melchers NVS, Stolk WA, Murdoch ME, et al. How does onchocerciasis-related skin and eye disease in Africa depend on cumulative exposure to infection and mass treatment? PLoS Negl Trop Dis 2021;15:e0009489.
7. WHO. Ouagadougou: African programme for onchocerciasis control, World Health Organisation Progress Report; 1st September 2009 - 31st August 2010. Available from: https://policycommons.net/artifacts/560404/the-world-health-organisation-year-2010-progress-report/1538180 [Last accessed on 29 Sep 2022].
8. Tchounkeu YF, Onyeneho NG, Wanji S, et al. Changes in stigma and discrimination of onchocerciasis in Africa. Trans R Soc Trop Med Hyg 2012;106:340-7.
9. Brieger WR, Frederick OO, Ososanya OO. Stigma associated with onchocercal skin disease among those affected near the Ofiki and Oyan rivers in western Nigeria. Soc Sci Med 1998;47:841-52.
10. Dana D, Debalke S, Mekonnen Z, et al. A community-based cross-sectional study of the epidemiology of onchocerciasis in unmapped villages for community directed treatment with ivermectin in Jimma Zone, southwestern Ethiopia. BMC Public Health 2015;15:595.
11. Cheke RA, Garms R. Indices of onchocerciasis transmission by different members of the Simulium damnosum complex conflict with the paradigm of forest and savanna parasite strains. Acta Trop 2013;125:43-52.
12. Yew YW, Kuan AHY, Ge L, Yap CWY, Heng BH. Psychosocial impact of skin disease: a population-based study. PLoS ONE 2020;15:e244765.
13. Crump A, Morel CM, Omura S. The onchocerciasis chronicle: from the beginning to the end? Trends Parasitol 2012;28:280-8.
14. Amazigo U. The African programme for onchocerciasis control (APOC). Ann Trop Med Parasitol 2008;102 Suppl 1:19-22.
15. Higazi TB, Geary TG, Mackenzie CD. Chemotherapy in the treatment, control, and elimination of human onchocerciasis. Res Rep Trop Med 2014;5:77-93.
16. Hotez PJ, Bottazzi ME, Zhan B, et al. The onchocerciasis vaccine for Africa - TOVA - initiative. PLoS Negl Trop Dis 2015;9:e0003422.
17. Kim YE, Remme JH, Steinmann P, Stolk WA, Roungou JB, Tediosi F. Correction: Control, elimination, and eradication of river blindness: scenarios, timelines, and ivermectin treatment needs in Africa. PLoS Negl Trop Dis 2015;9:e0003777.
18. Ozoh GA, Murdoch ME, Bissek A-C, Hagan M, et al. The African programme for onchocerciasis control: impact on onchocercal skin disease. Trop Med & Intl Hlth 2011;16:875-83.
19. Noma M, Zouré HGM, Tekle AH, et al. The geographic distribution of onchocerciasis in the 20 participating countries of the African programme for onchocerciasis control: (1) priority areas for ivermectin treatment. Parasit Vectors 2014;7:325.
20. Alonso LM, Murdoch ME, Jofre-Bonet M. Psychosocial and economic evaluation of onchocerciasis: a literature review. Soc Med 2009;4:8-31.
21. Wagbatsoma VA, Okojie OH. Psychosocial effects of river blindness in a rural community in Nigeria. J R Soc Promot Health 2004;124:134-6.
22. Okoye IC, Onwuliri CO. Epidemiology and psycho-social aspects of onchocercal skin diseases in northeastern Nigeria. Filaria J 2007;6:15.
23. Gemade EI, Utsalo SJ. Onchocerciasis in Benue State Nigeria. VI. The prevalence and distribution of the disease among the human population in Sati-kiyo village. Act Leiden 1990;59:51-8.
24. Worth C, Heukelbach J, Fengler G, Walter B, Liesenfeld O, Feldmeier H. Impaired quality of life in adults and children with scabies from an impoverished community in Brazil. Int J Dermatol 2012;51:275-82.
25. WHO. Methods for community diagnosis of Onchocerciasis to guide ivermectin based control in Africa. WHO report of an informal consultation held in Ougadougou, November 19-21,1991. Available from:https://apps.who.int/iris/handle/10665/204268 [Last accessed on 29 Sep 2022].
26. Murdoch ME, Hay RJ, Mackenzie CD, et al. A clinical classification and grading system of the cutaneous changes in onchocerciasis. Br J Dermatol 1993;129:260-9.
27. Onekutu A, Ayom F, Iboyi M. Prevalence and Distribution of Human Onchocerciasis and Dermatological Features in Kwande Local Government Area of Benue State, Nigeria. JAMMR 2018;27:1-10.
28. Otabil KB, Gyasi SF, Awuah E, et al. Prevalence of onchocerciasis and associated clinical manifestations in selected hypoendemic communities in Ghana following long-term administration of ivermectin. BMC Infect Dis 2019;19:431.
30. Remme JHF. The global burden of onchocerciasis in 1990. Available from: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.177.9964&rep=rep1&type=pdf [Last accessed on 26 Sep 2022].
31. Kifle B, Woldemichael K, Nigatu M. Prevalence of Onchocerciasis and Associated Factors among Adults Aged ≥ 15 Years in Semen Bench District, Bench Maji Zone, Southwest Ethiopia: Community Based Cross-Sectional Study. Adv Public Health 2019;2019:1-9.
32. Oladipo O, Brieger WR, Otusanya S, Kale OO, Offiong S, et al. Farm land size and onchocerciasis status of peasant farmers in southwestern Nigeria. Trop Med & Inter Hlth ;1997:334-40.
33. Adewale B, Oyerinde JPO, Mafe MA. Seasonal biting pattern of Simulium damnosum s.l and its implications on onchocerciasis treatment with ivermectin. W Afr J Med 2008;27:224-9.
34. Adeleke MA, Mafiana CF, Sam-wobo SO, et al. Biting behaviour of Simulium damnosum complex and Onchocerca volvulus infection along the Osun River, Southwest Nigeria. Parasit Vect 2010;3:93.
35. Domche A, Nana-Djeunga HC, Yemeli LD, et al. Knowledge/perception and attitude/practices of populations of two first-line communities of the Centre Region of Cameroon regarding onchocerciasis and black fly nuisance and bio-ecology. Parasit Vectors 2021;14:546.
36. Ugbomoiko US Dalumo V, Danladi YK, Ofoeze IE, Heukelbach J. Concurrent urinary and intestinal schistosomiasis and intestinal helminthic infections in schoolchildren in Ilobu, South-western Nigeria. Acta Trop 2012;123:16-21.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Ugbomoiko US, Bem A, Babamale AO, Adegbola RQ, Amase N, Alencar CH, Heukelbach J. Onchocercal skin disease in Benue state, Nigeria: integrated assessment of burden and psychosocial impact, and associated factors. One Health Implement Res 2022;2:108-20. http://dx.doi.org/10.20517/ohir.2022.11
AMA Style
Ugbomoiko US, Bem A, Babamale AO, Adegbola RQ, Amase N, Alencar CH, Heukelbach J. Onchocercal skin disease in Benue state, Nigeria: integrated assessment of burden and psychosocial impact, and associated factors. One Health & Implementation Research. 2022; 2(4): 108-20. http://dx.doi.org/10.20517/ohir.2022.11
Chicago/Turabian Style
Ugbomoiko, Uade Samuel, Asen Bem, Abdulkareen Olarewaju Babamale, Rukayat Queen Adegbola, Nyamngee Amase, Carlos Henrique Alencar, Jorg Heukelbach. 2022. "Onchocercal skin disease in Benue state, Nigeria: integrated assessment of burden and psychosocial impact, and associated factors" One Health & Implementation Research. 2, no.4: 108-20. http://dx.doi.org/10.20517/ohir.2022.11
ACS Style
Ugbomoiko, US.; Bem A.; Babamale AO.; Adegbola RQ.; Amase N.; Alencar CH.; Heukelbach J. Onchocercal skin disease in Benue state, Nigeria: integrated assessment of burden and psychosocial impact, and associated factors. One. Health Implement. Res. 2022, 2, 108-20. http://dx.doi.org/10.20517/ohir.2022.11
About This Article
Copyright
Data & Comments
Data

 Cite This Article 16 clicks
Cite This Article 16 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.